Glaucoma, a leading cause of blindness, can sneak
 Berlin - You are sitting in a bus and suddenly the person beside you disappears from your visual field. Or the far end of the pencil on the corner of the desk in front of you fades into black. These and similar visual disturbances could be signs of glaucoma.
Berlin - You are sitting in a bus and suddenly the person beside you disappears from your visual field. Or the far end of the pencil on the corner of the desk in front of you fades into black. These and similar visual disturbances could be signs of glaucoma.
One of the most frequent causes of blindness, glaucoma may slowly cause damage to nerve cells in the retina and optic nerve. By the time symptoms appear, it is often already too late.
Elevated pressure within the eye was long thought to cause glaucoma. "We now know this is merely a risk factor, albeit a very significant one," noted Ronald Gerste, an opthamologist and the general secretary of the Initiative for Early Detection of Glaucoma in the German town of Germering.
Another common cause of cell damage is insufficient or fluctuating blood circulation in the eye. "Increased intraocular pressure is very often associated with low or fluctuating blood pressure," Gerste said.
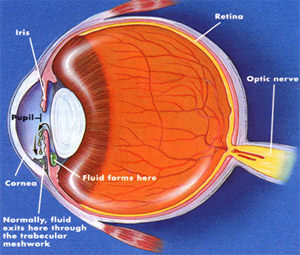
A watery fluid called aqueous humour is constantly produced inside the eyeball. It nourishes the cornea and lens and maintains the convex shape of the former. In a healthy eye, production and drainage of aqueous humour occur at equal rates. Drainage can be impeded, however, by blockage due to deposits, deformity or inflammation.
An injury, congenital developmental disorder or diabetes could also be to blame. The result is increased pressure on the optic nerve, squeezing the sensitive cells.
Glaucoma is an insidious disorder because the eye can compensate for the damage for a long time without impaired function. "By the time an affected person notices changes in vision, 30 to 40 per cent of the nerve cells have already been destroyed," remarked Helga Kipp of the Dortmund-based branch of the National Glaucoma Self-Help Association.
"At that point," she said, "central vision is already obscured, irreparable damage has been done and the only thing that one can do is to try to preserve what is left intact therapeutically."
The main treatment for glaucoma is to lower intraocular pressure with eye drops. "Patients used to complain primarily about the burning sensation caused by the drops," noted Georg Eckert, spokesman for the Opthamological Association of Germany. "The drops also dilated the pupils, which patients subjectively experienced as worsening their vision."
Today's eye drops, however, are far less unpleasant and more effective, Eckert said.
Nevertheless, modern glaucoma treatment involves a certain degree of inconvenience. "You've got to take the eye drops with you everywhere," Kipp said. "Some patients suffer from side effects such as eye pain, cough and the discharge of mucous." Elderly patients and people with arthritic fingers have particular difficulty putting in the eye drops.
For reasons such as these, some patients neglect treatment, especially in glaucoma's early stages when visual impairment is slight or still imperceptible. "That's a serious mistake," warned Eckert, who said progression of the eye disorder could be arrested only by continual treatment and regular examinations.
The other method of treatment, namely surgery, is chosen in no more than 10 to 20 per cent of glaucoma cases. The advantage of surgery, Gerste said, is that "a single operation can lower pressure within the eye much more than is possible with eye drops." What is more, the quality of the patient's everyday life is not affected.
The patient must weigh the respective risks and benefits of treatment methods together with his or her doctor. "It's essential to get a second opinion, for example in an eye clinic," Kipp pointed out.
Since any treatment can preserve no more than the visual faculty extant when treatment starts, experts recommend early-detection examinations beginning at age 40 at the latest. The eye doctor then measures intraocular pressure and visual field, does a thorough check of the optic nerve - looking, for example, for possible damage around the edges - and may produce images of the optic nerve head.
The doctor must also determine whether the patient has any personal risk factors such as low or fluctuating blood pressure, cardiovascular disease, insufficient cornea thickness, diabetes or a family history of glaucoma. (dpa)